A Comprehensive Guide to Breast Milk Production
Share
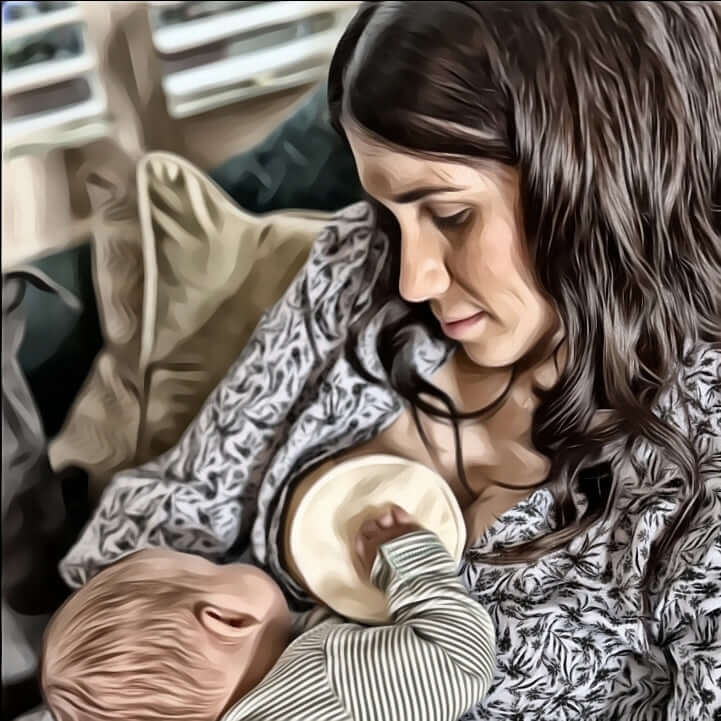
Breastfeeding is a unique and precious bonding experience between you and your baby, providing numerous health benefits for both of you. Understanding the anatomy, physiology, and hormonal regulation of breast milk production can empower you to optimize your milk supply.
Anatomy and Physiology of the Breast
1.1 Structure of the Breast:
The breast is composed of glandular tissue, which consists of lobes, ducts, and milk-producing glands. Each breast contains multiple lobes that are further divided into smaller lobules. Within these lobules are clusters of milk-producing glands called alveoli, where milk synthesis occurs (1).
1.2 The Role of the Nipple and Areola:
The nipple and areola play crucial roles in breastfeeding. The nipple is the raised projection through which the milk is released. Surrounding the nipple, the areola contains small bumps called Montgomery glands, which secrete protective oils to moisturize and safeguard the skin during breastfeeding (2).
1.3 Proper Latch and Positioning:
Achieving a proper latch and positioning is essential for effective milk transfer and preventing discomfort. Ensuring that your baby's mouth covers not only the nipple but also a significant portion of the areola promotes efficient milk extraction. Seek guidance from lactation consultants or healthcare providers to assist you in mastering this skill.
Hormonal Regulation of Milk Production
2.1 Prolactin:
Prolactin is a hormone produced in the pituitary gland that plays a central role in milk production. During pregnancy, rising levels of prolactin prepare the breasts for milk synthesis. After birth, suckling stimulates the release of prolactin, signaling the mammary glands to produce milk (3).
2.2 Oxytocin:
Oxytocin, often referred to as the "love hormone," triggers the letdown reflex, enabling milk to flow from the alveoli through the milk ducts to the nipple. Oxytocin is released in response to your baby's sucking or a mechanical stimulus, such as a breast pump. It also contributes to the bonding and relaxation experienced during breastfeeding (4).
2.3 Supply and Demand:
Breast milk production operates on the principle of supply and demand. Frequent and effective milk removal stimulates the breasts to produce more milk. The more often milk is removed, the more milk the breasts will make to meet your baby's needs. Establishing a consistent breastfeeding or pumping routine helps maintain an ample milk supply.
Process of Milk Production
3.1 Stimulation of Nerves:
The process of milk production begins with the stimulation of nerves in the breast, triggered by your baby's suckling or breast pumping. These nerve signals transmit a message to the hypothalamus, a region in the brain, which releases prolactin and oxytocin (5).
3.2 Milk Syntheies:
Once prolactin is released, it travels through your bloodstream to the mammary glands, where it stimulates the alveoli to start producing milk. Specialized cells within the alveoli take up components from your blood, such as proteins, sugars, and fats, to create breast milk (6).
3.3 Milk Letdown:
The release of oxytocin, triggered by suckling or mechanical stimulation, causes the milk to be squeezed out of the alveoli and into the milk ducts. This process is known as milk letdown or the milk-ejection reflex. The milk is then available for your baby to consume during breastfeeding or can be expressed using a breast pump (7).
Understanding the intricate processes involved in breast milk production can help you navigate your breastfeeding journey more confidently. Remember to seek guidance from lactation consultants or healthcare providers for personalized advice. For additional visual aids and infographics, visit reputable sources such as the CDC or AAP websites, where you can find useful resources to enhance your understanding of breastfeeding and breast milk production.
References:
- American Academy of Pediatrics. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841.
- American Academy of Pediatrics. (2015). New Mother’s Guide to Breastfeeding (3rd ed.). Elk Grove Village, IL: American Academy of Pediatrics.
- Neville, M. C., & Morton, J. (2001). Physiology and endocrine changes underlying human lactogenesis II. Journal of Nutrition, 131(11), 3005S–3008S.
- Uvnäs-Moberg, K. (2012). Oxytocin: The hormone of love and bonding. Journal of Child and Adolescent Psychopharmacology, 22(1), 11–18.
- Stuebe, A. M. (2012). The risks of not breastfeeding for mothers and infants. Reviews in Obstetrics and Gynecology, 5(4), 222–231.
- Oftedal, O. T. (2002). The evolution of milk secretion and its ancient origins. Animal, 412-425.
- Meier, P. P., Engstrom, J. L., Patel, A. L., Jegier, B. J., Bruns, N. E., & Baird, D. C. (2010). Improving the use of human milk during and after the NICU stay. Clinics in Perinatology, 37(1), 217–245.

